The invention of the Left Ventricular Assist Device (LVAD) to manage and treat chronic cardiovascular conditions like heart failure, marked a pivotal moment in medical and healthcare advancement. To date, heart failure remains one of the most difficult health conditions due to the high rate of mortality it leaves in its wake. Heart failures can be quite severe, and the almost non-existent chance of survival without a heart transplant or implantation of heart-assisted devices like LVAD makes the illness all the more terrifying.

Whenever people hear the term ‘heart failure’, it sends shivers down their spine because this could mean a shorter than expected lifespan for them or their loved ones diagnosed with the illness. In cases where people have the chance of surviving severe heart failure, this could mean an exhausting road ahead, filled with hospital visits and an indefinite wait for compatible donor hearts. However, since the debut of the Left Ventricular Assist Device, LVAD on the medical scene, some remarkable progress has been made in prolonging lives by managing the conditions of people whose hearts are incapable of functioning at the normal capacity of a healthy human heart.
A Brief History and Overview of LVAD
The human heart has four chambers, the Left Ventricle is one of them. Each chamber serves a different purpose in regulating the flow of blood and, located at the bottom of the heart, the left ventricle is responsible for pumping and circulating oxygen-rich blood into vital organs and other parts of the body. When this chamber becomes too weak to carry out its function, heart failure is inevitable. For this reason, the LVAD was invented to take pressure off a weak left ventricle and assist it in performing its function.
LVAD is an artificial heart pump that is implanted in the chest to help a weakened or failing heart pump and circulate blood as a normally functioning heart would. Its history can be traced back to the 1960s when Dr. Michael DeBakey, a vascular and cardiac surgeon, and pioneer in the development of artificial heart, performed the first-ever successful LVAD implantation surgery on a 37-year woman, who was dealing with heart failure. The Left Ventricular Assist Device was able to sustain the patient for the ten days until her heart transplant surgery.

The early LVAD consisted of a titanium frame and a polyurethane pump, powered by compressed air or gas. However, advancements in medical innovations and procedures have led to improvements in LVADs and the creation of the Novacor pump and the HeartMate XVE pump. Continuous strides in heart failure treatment also made room for the launch of HeartMate II and HeartMate III, which are clinically approved for managing conditions of patients with varying degrees of heart failure.
How LVAD Functions as an Artificial Heart Pump
So many people suffering from heart failure depend heavily on LVADs to stay alive, and the technology has proven to be reliable so far. However, as much as this device performs a major heart function, it does not in any way replace the human heart. It is just an assistant that pumps alongside the patient’s heart. The LVAD receives blood from the left ventricle and delivers it to the aorta, the main artery that transports blood from the heart to the rest of the body.
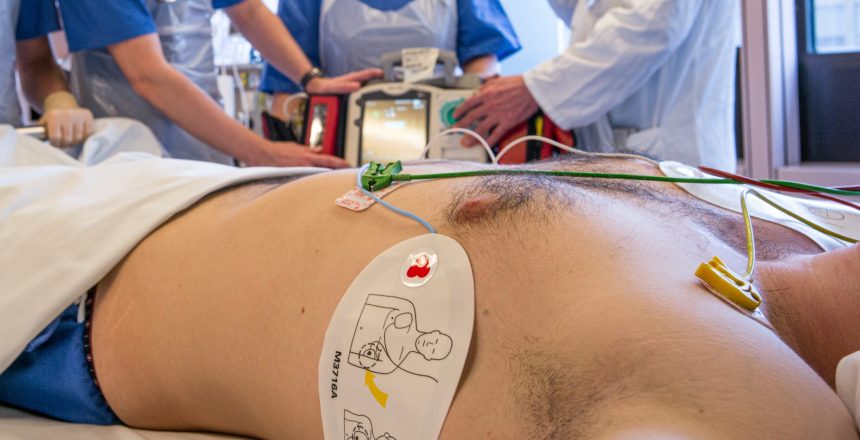
Implantation of an LVAD requires open-heart surgery, where the surgeon makes a long incision in the breastbone, spreading the rib cage to access the heart. The LVAD pump is then fixed into the apex of the heart where it receives blood and delivers this blood through a connecting tube to the aorta. The device is then attached to a cable referred to as a driveline, and a controller that helps the patient to operate the pump properly. The driveline is passed through the skin on the stomach to the controller on the outer part of the patient’s body.
This artificial heart pump is powered by batteries that can be charged through a cord that plugs into an electrical socket. When the battery begins to run low, the controller alerts the patient. Also, all LVAD controllers have a spare battery, so when one runs down, the other powers the LVAD for several more hours. In addition, the controller has standby circuitry configured to pick up if the primary circuitry fails.
The LVAD Journey So Far: Milestones and Pitfalls
Heart failure treatment has really progressed over the years and more individuals suffering from varying stages of heart failure can now benefit from LVAD implantation. One group of individuals that have benefitted greatly from LVADs since its inception are those waiting for a heart transplant but who have extremely weak hearts, incapable of keeping them alive while they await a compatible donor heart. In this instance, the use of LVAD is classified as a ‘Bridge to Transplant.’
Another category of people who benefit from this technology is those recovering from cardiovascular issues like heart attacks, cardiac surgery, or open-heart surgery, whose hearts need rest. In the last decade, an additional category of people who began benefiting from LVAD implantation were patients with heart failure who are not viable candidates for a heart transplant. In cases like this, the artificial pump is implanted to boost the patients’ cardiovascular function for the rest of their lives. In situations like this, the use of LVAD is classified as ‘Destination Therapy.’

Today, the cardiology sphere has recorded an impressive number of heart failure patients enjoying an improved quality of life following their LVAD implantation surgery. The life expectancy of heart failure patients without an LVAD implantation is usually a year or less, but patients with LVAD are expected to stay alive for up to five years. However, with the new generation LVADs, some patients have lived up to 13 vibrant years after the surgery, which is a major feat in heart failure therapy.
Despite the hope surrounding the progress made with LVAD, It is important to note that every medical procedure comes with huge risks and LVAD implantation is no exception. The possible risks from LVAD implantation include device malfunction, stroke, right heart failure, blood clots, internal bleeding, blood cell damage, infections, and some other health threats. It is for this reason that a thorough total body evaluation is carried out on heart failure patients to determine those who are good candidates for the treatment. Nonetheless, even viable candidates for the surgery are still at risk of developing complications after the LVAD implantation.
What Does the Future Hold for LVAD Therapy?
Compared to where it was several decades ago, the medical and healthcare field has grown by leaps and bounds, owing to technological influence on the treatment and management of a wide range of ailments and health conditions. Cardiology has profited greatly from this with the continued development of LVAD therapy. The remarkable transformation of LVADs through the years is proof that progress in the treatment of cardiovascular health conditions has remained on an upward trajectory.
HeartMate II, which is a new generation LVAD, is now implanted for short and long durations in more patients with both intermediate and advanced levels of heart failure. Also, HeartMate III, the most recent in the HeartMate series, was approved a few years back as a long-term solution for patients with advanced heart failure and who are not candidates for a heart transplant. This is a further indication that there is likely more to come in heart failure treatment and management.
As science and technological innovations help experts break more ground in the medical field, there are great chances of the development of wireless LVADs in years to come. Could this also mean the future holds the possibility of an LVAD becoming an alternative to a heart transplant? We will just have to wait to find out.
Enjoyed this article? Visit the 4P Academy Blog for more informative pieces on a variety of fascinating topics.