The COVID 19 pandemic has placed much of our society’s spotlight on science and immunological research, with the talk of vaccines leading topical issues across the globe. Before the pandemic, only researchers knew what a Polymerase Chain Reaction assay (PCR) could do, and now? A lot more people have become familiar with the term PCR and its use in testing for viral DNA. With the ravaging impact of COVID 19, so many companies, health ministries, scientists, and news agencies have been working tirelessly to make scientific discoveries and research undertakings revolving around the pandemic accessible to the general public. While presenting facts gained by science remains a step in the right direction, it is also important that researchers highlight the science behind those facts for educative purposes. In the case of vaccines, which take priority spot in pandemic science, the best way to understand how they work is to examine the history of their development.
A Brief Overview of the Human Immune System
The immune system has two main parts: the innate and the adaptive immune system. Our innate immune system is a sort of prevention system. It is, however, important to know that it does not develop or grow smarter in the same way that the adaptive immune system does. The innate immune system includes barriers such as our skin or nose hairs to keep pathogens out and serve as the body’s first line of defence. Nevertheless, should pathogens find their way into our bodies, the innate immune system is prepared. Our cells feature receptors on their surface, which act like ‘ticket-checkers at a concert. If something tries to enter a cell without the right ticket (or, in this case, the right protein attached to it), it can’t gain entrance.
Likewise, some receptors act like ‘bag checkers so that no one brings anything dangerous into the concert. These receptors are on macrophages, neutrophils, and eosinophils (white blood cells). They are specifically designed to produce a signal if one of many easily recognizable pathogenic structures is attached. Neutrophils are more abundant than other white blood cells, and they can identify microbes such as bacteria or fungi. Eosinophils are less common but very important due to their ability to identify and kill parasites, too large for other immune cells to fight against.
Macrophages are the most general of the white blood cells, able to target a variety of pathogens, in addition to breaking down dead cells. Furthermore, they are significant for activating the adaptive portion of our immune system. The innate immune system is built to work quickly and on anything that our cells deem ‘not quite right,’ but lacks some essential features. Nevertheless, the adaptive immune system makes up for whatever features the innate immune system lacks. First, the adaptive immune system can target specific pathogens, which is important if the body develops a widespread infection. It also serves as the immune system’s memory that takes the initiative to produce cells designed to attack a specific pathogen your body has successfully fought off if it should ever show up again.
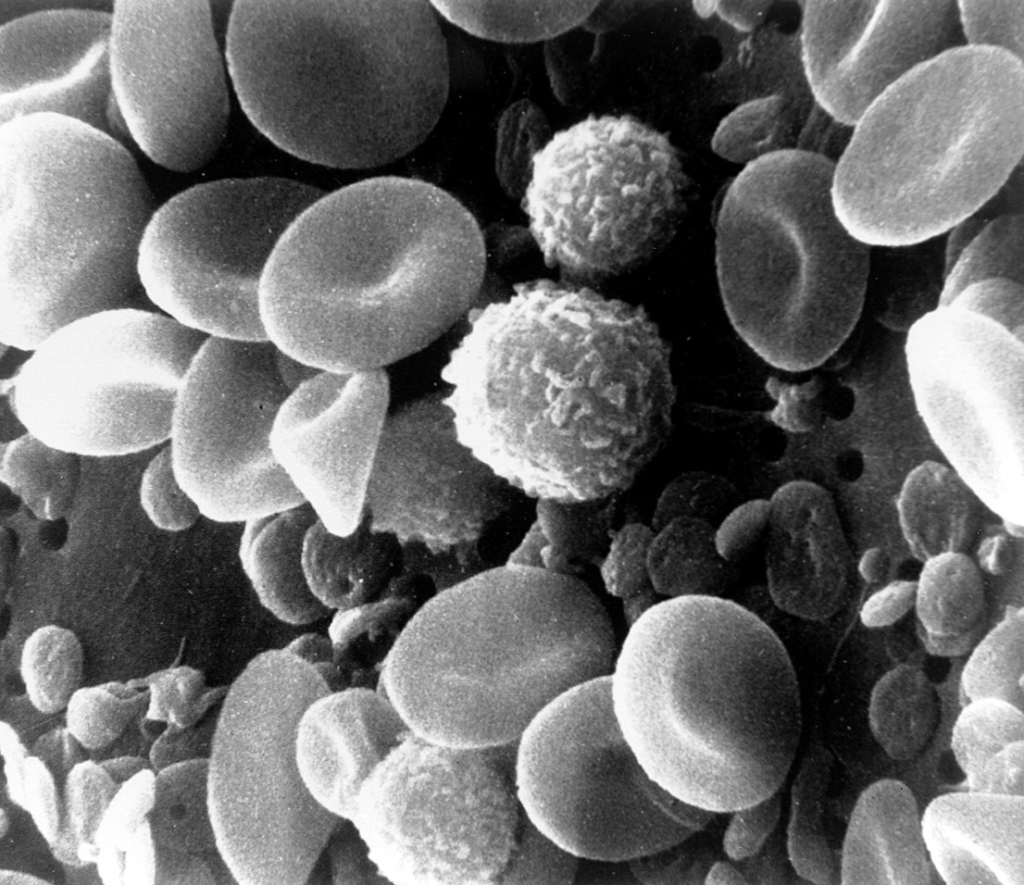
The adaptive immune system is composed of lymphocytes, yet another type of white blood cell. Lymphocytes produce B cells and T cells. B cells go on to produce antibodies, which are proteins built to attach to a specific pathogen. These cells, which can be produced in large numbers, prevent the pathogen from subduing our ‘ticket-checkers in the innate immune system and mark the pathogen so that a white blood cell can identify and destroy it.
On the other hand, T cells can identify which of our cells have been infected. An infected cell will eventually break open and release a large amount of the pathogen that infected it. So, the job of the T cell is to either destroy the cell before that happens or tell the cell to fight back. T cells can also warn the neighbours of the infected cell to stay alert and ward off the pathogen when it attempts to enter.
Situations Where a Vaccine Can Help, and How They Do It
The immune system is truly remarkable, but sometimes a pathogen comes along that it just can’t keep up with. In such situations, the innate immune system does not recognize the pathogen, and the adaptive immune system cannot work quickly enough to stop the infection, and soon the body is overwhelmed. Vaccines are the best way to prevent cases such as this. Vaccines do not affect the innate immune system, but they can teach your adaptive immune system to identify and destroy a specific pathogen. One might ask, how does a vaccine accomplish this? We can uncover the answer by examining the major milestones in vaccine development.
Variolation and Smallpox: The 1600s
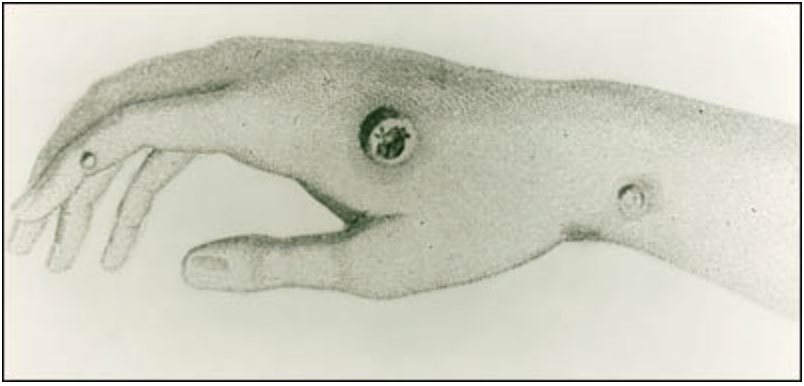
The first form of vaccination to be used as a process is called variolation. This process involved taking a small amount of an infected person’s fluids (usually blood or pus) and applying that to a small open wound on a healthy person. This form of vaccine came about due to the smallpox virus, Variola vera. Smallpox was extremely transmissible, with symptoms including fever, headache, back pain, and the eventual development of raised pus-filled sores (pocks).
The idea behind variolation dates back to 430 BC, when medical scientists discovered that smallpox survivors could not contract it again. As such, they appointed these survivors as caregivers to those infected with it. This eventually led to variolation, which became widespread across Asia, Africa, and Europe by the mid to late 1600s. Variolation works by introducing to the body a tiny amount of the pathogen. This gives your immune system enough time to respond instead of immediately becoming overwhelmed. That said, variolation was not without its problems. About one in every 50 people who received this form of vaccination would cause a new outbreak or die from the illness.
Edward Jenner and the First Smallpox Vaccine: 1796
Edward Jenner is famously known as the first person to create a vaccine. While variolation was simply exposing the body to a small amount of the pathogen and then hoping for the best, Jenner’s vaccine did something similar, but with one key difference. Jenner was a medical doctor who researched the properties of blood. He had heard something interesting about milkmaids being immune to smallpox. This piece of information at first might have sounded to him like an odd bit of superstition. However, after investigating the subject, he found that milkmaids were indeed immune to smallpox, but only after being exposed to cowpox from their herd.
So in 1796, Jenner collected a cowpox sample from a milkmaid by the name of Sarah Nelms and injected James Phipps, an 8-year-old boy, with it. He recorded that James fell ill with a mild fever and would occasionally lose his appetite. The boy experienced no symptoms whatsoever! Nine days after his injection with cowpox, James was fully recovered, and Jenner injected him with smallpox. Although it took a few years after this experiment for the process to become an accepted way to immunize people against smallpox, it eventually became a revolutionary discovery. Jenner named his procedure after the Latin word for cowpox, vaccinia, calling it a Vaccination.
Louis Pasteur and the First Live Attenuated Vaccine: 1897
The name Louis Pasteur might be one you recognize for his role in coining the term pasteurization, from a process he discovered where milk is heated and cooled to kill any microbes present in the product. He, however, has a crucial place in the history of vaccines as well for developing one of the first live attenuated vaccines in the 1880s and 90s. The vaccine was for cholera, a bacterial infection that causes severe diarrhea responsible for rapid dehydration and death.
Pasteur discovered that, by growing the bacteria in culture (a jelly-like plate of microbe food) and transferring the weakest colonies to new plates every so often, eventually, you could produce a pathogen only capable of surviving in the most coddled of conditions (i.e. the culture). Pasteur did not know why this process weakened the bacteria, but it did, and injecting chickens with it led to their immunity to cholera. Nonetheless, his discovery revealed that growing pathogens for long periods in culture provides ample time for random mutations.
Viruses and bacteria are built to develop mutations at a high frequency. This predisposition and their small single-celled structure increase the possibility of developing a mutation that will allow the pathogen to be better at survival. This has led to problems like bacteria becoming resistant to antibiotics or the many variants we see of COVID-19, but it has also enabled the production of vaccines. This method is so effective that attenuated vaccines are still used today for many common viruses such as measles, mumps, yellow fever, and some influenzas.

However, you may wonder how scientists are sure that a pathogen will grow weaker than stronger through mutations in the live attenuation process? Well, when scientists grow pathogens in a culture that gives them everything they need and makes the pathogen’s life super easy, it gets lazier and lazier over the course of many generations. This is because survival mutations help pathogens survive, but they also use up a lot of energy, so if they aren’t needed, it becomes more beneficial for a pathogen not to have them.
Development of Bacterial Vaccines: 1890 – 1950
Interestingly in modern medicine, live attenuated vaccines are used almost solely to vaccinate against viruses and not against bacteria. This is because of the somewhat unpredictable nature of attenuation. Viruses have tiny genomes, making them fairly easy to attenuate and to maintain product safety. Compared to viruses, bacteria have massive genomes, not to mention viruses and pathogens of their own, so there are often too many variables to produce an attenuated bacterial vaccine safely. The genomes in bacteria are so complex that, unlike viruses, it is nearly impossible to know what every one of their genes does.
So, after Louis Pasteur’s amazing discovery, vaccines took off, and scientists all over the world started attempting to make them. Viral vaccines came along quickly, but unlike Pasteur, other scientists had far less luck making effective vaccines against bacteria. It wasn’t until the 1950s and onwards, when genetics advanced, that live attenuated bacterial vaccines became possible.
Still, it is unlikely that you will receive a live attenuated bacterial vaccine because they are often just too complex to ensure their safety. It is difficult to say if they will result in consistent immunity. That said, this only explains why there are so few of them; live attenuated vaccines are still often used for well-studied bacterial diseases such as typhoid (caused by salmonella), and these are very safe.
COVID Pandemic: The Two Main Types of COVID 19 Vaccines in North America
Today, the world as a whole has a better appreciation for vaccines following the rise and rapid spread of SARS CoV2, a viral infection that has resulted in the illness called COVID 19. Now, with the increased availability of COVID vaccines thanks to the efforts of researchers and scientists, there is some hope that we are approaching the light at the end of the tunnel. The availability of these vaccines and, by extension, all the history behind the development of vaccines make the end of this pandemic possible.
Presently in North America, there are two types of vaccines available to help our bodies combat these infections. The first is the mRNA vaccine, produced by Moderna and Pfizer, respectively. To understand this vaccine, it’s important first to understand mRNA. DNA stands for deoxyribonucleic acid. This is a molecule built-in two twisting strands that are used to store instructions on how to build any living thing, including us humans. These instructions are referred to as a genome, and a copy of your genome is present in every one of your cells (except for red blood cells and platelets).
RNA becomes important when your cells need to read their instructions and create the parts as instructed. Our DNA is very delicate, so it is hidden away in a cell’s nucleus, where most of the cell’s construction equipment can’t touch it. Instead, the nucleus has special machinery to gently separate small sections of DNA and copy only the instructions your cells need. They ‘write down’ these instructions in the form of single-stranded RNA. RNA stands for ribonucleic acid, and there are many different types of it. The kind, however, that carries these instructions is called mRNA, where the m stands for messenger.
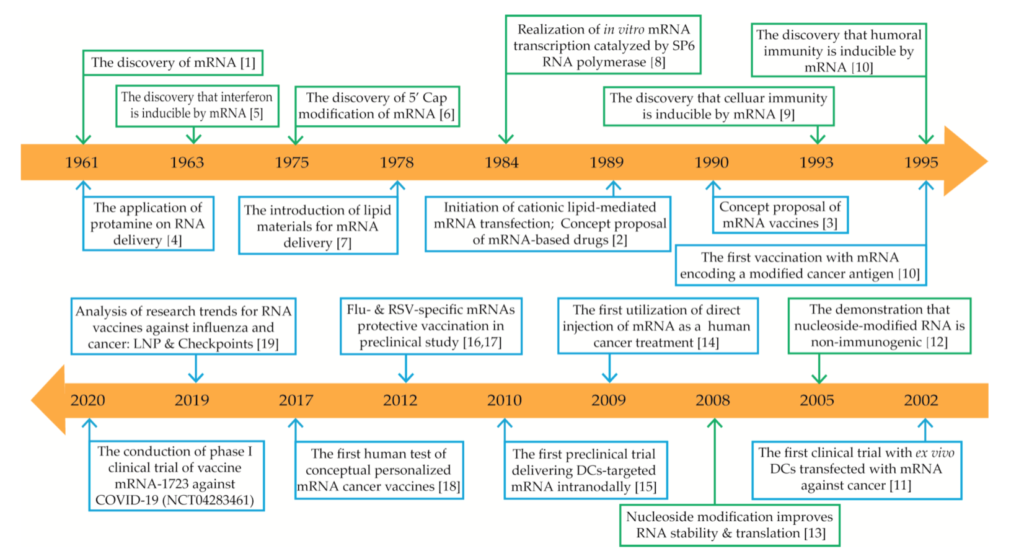
mRNA vaccines pump you (and, by extension, your cells) with the mRNA instructions to make only one part of the virus. Specifically, it will make a part of the virus that can be recognized by your adaptive immune system so that your B cells will learn to produce antibodies able to mark the virus for destruction. A good way to look at this is by using a metaphorical analogy. If the virus is an army that has come to invade your territory (body), then the mRNA vaccine shows you the flag that the army carries to help identify the army when it approaches.
Next is the adenoviral vaccine, the type which Johnson & Johnson and Astra Zeneca produce. This vaccine is also referred to as a viral vector vaccine. It uses a harmless virus as a vessel to deliver DNA to your cells. This DNA codes for a particular part of the virus, similarly to mRNA vaccines. Your cells will build that harmless protein ‘flag’ based on the DNA instructions, and your body learns to recognize this specific enemy.
The virus used to deliver the DNA will vary depending on the brand of vaccine being administered, but the key thing to know is that these are not viruses in the traditional sense of the word. When doing genetic research, scientists frequently use viruses as a way to interact with cells. This is because our cells don’t let in just anything. We have those ‘ticket-checkers receptors on all our cells, and if you don’t have a ticket or if your ticket looks like counterfeit, then you don’t get in.
It is hard to design a fake ticket, or in this case, a complex protein structure, so instead, scientists use viruses that have already made themselves some fake tickets. These viruses can be thought of like a pill capsule, and they have been emptied of everything they contain (meaning the bad stuff). These empty viral vectors can then be filled with the DNA that codes for the enemy flag. In other words, the virus portion of adenoviral vaccines is used as a shell that contains a vaccine in it.
Dispelling a Misunderstanding
An important thing to know about the two broad types of vaccines being used in the USA and Canada is that, though these vaccines utilize genetic code (mRNA and DNA), they cannot alter your genes or your genome by extension. None of the vaccines being used to fight COVID 19 can alter your genes, but since we’ve focused our discussion on North American vaccination, I want to continue in that thread. Earlier, I noted that your genome is stored inside each cell’s nucleus and that the nucleus doesn’t let very much in; that includes foreign genetic material. If something can’t enter the nucleus, then it can’t be inserted into your genome.
Finally, this blog article synthesizes some truly amazing research works that you can read up on if you want more information about this topic. Unfortunately, scientific research is not always an easy read, so to make life a bit easier, I recommend reading the abstract and conclusion (also sometimes titled discussion) sections and looking at the introduction for additional background information on the subject matter. Should you have burning questions about vaccines that this article or those cited here did not highlight, consider reaching out to a trusted expert in science or healthcare for their thoughts or advice.
Enjoyed this article? Visit the 4P Academy Blog for more informative pieces on a variety of fascinating topics.
SOURCES
Alberts B, Johnson A, Lewis J, et al. Molecular Biology of the Cell. 4th edition. New York: Garland Science; 2002. Chapter 24, The Adaptive Immune System..https://www.ncbi.nlm.nih.gov/books/NBK21070/
Alberts B, Johnson A, Lewis J, et al. Molecular Biology of the Cell. 4th edition. New York: Garland Science; 2002. Innate Immunity. https://www.ncbi.nlm.nih.gov/books/NBK26846/
Pasteur, L. The attenuation of the causal agent of fowl cholera. Comptes rendus de l’Academie des sciences. 1880. (91), 673-680. http://icwdm.org/wp-content/uploads/2016/06/fowlcholerapasteur.pdf
Riedel, S. Edward Jenner and the History of Smallpox and Vaccination. Proceedings – Baylor University. Medical Center. 2005. 18(1), 21–25. https://doi.org/10.1080/08998280.2005.11928028
Schlake, T., Thess, A., Fortin-Mleczek, M, et al. Developing mRNA-vaccine technologies. RNA Biology, 2012. 9(11), 1319–1330. https://doi.org/10.4161/rna.22269
Smith, A. Louis Pasteur, the father of immunology? Frontiers in Immunology. 2012. 3, 68–68. https://doi.org/10.3389/fimmu.2012.00068
Surat, P. What is the difference between a phagocyte, macrophage, neutrophil, and eosinophil? News-Medical. https://www.news-medical.net/life-sciences/What-is-the-difference-Between-a-Phagocyte-Macrophage-Neutrophil-and-Eosinophil.aspx
Zepp, F. Principles of Vaccination. Vaccine Design, 1403, 57–84. 2016. https://doi.org/10.1007/978-1-4939-3387-7_3
PICTURE SOURCE
Xu, S, Yang, K. Li, R., et al. mRNA vaccine era—Mechanisms, drug platform and clinical prospection. Int. J. Mol. Sci. 2020, (21). https://doi.org/10.3390/ijms21186582

